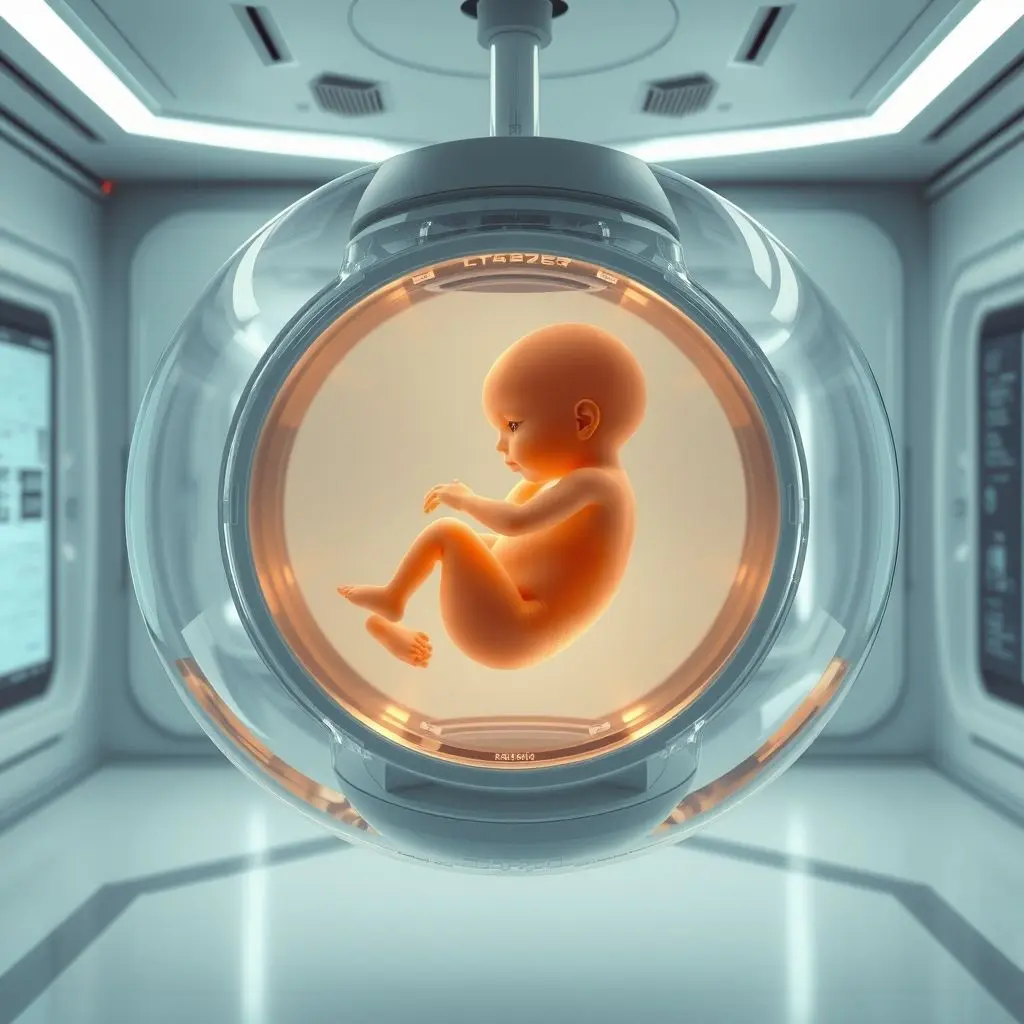
Picture a future where the gentle hum of a machine replaces the rhythmic beat within a human body, nurturing new life. A world where infants gestate not inside a person, but within an external, artificial environment. It sounds like a concept ripped straight from the pages of a science fiction novel, right? Yet, this isn’t mere fantasy; the groundbreaking science behind it is already making incredible strides.
While a fully functioning artificial womb for human gestation from conception is still a distant horizon, the underlying technology is very real and currently deployed in critical care settings. Researchers are utilizing sophisticated systems to mimic the natural uterine environment, providing a lifeline for extremely premature infants – those born far too early to survive outside the womb under conventional means. This cutting-edge field, often dubbed ectogenesis, holds immense potential, hinting at a future where the very definition of pregnancy and birth could be dramatically redefined.
Before we dive deeper into the profound implications of this technology, take a moment to visualize this mind-bending possibility. We’ve captured some of these ideas in a short video. Give it a watch!
Table of Contents
Beyond Sci-Fi: The Current State of Artificial Wombs
The term “artificial womb” might conjure images of futuristic pods, but today’s reality is more focused and medically driven. The most significant progress has been made in supporting extremely premature infants, specifically those born at the very edge of viability, often between 22 and 24 weeks gestation. These babies face immense challenges; their lungs, brains, and other vital organs are critically underdeveloped.
Traditional neonatal intensive care units (NICUs) rely on ventilators, incubators, and complex medical interventions. While life-saving, these methods can still cause long-term complications for these fragile infants. An artificial womb offers a different approach: simulating the fluid-filled, low-pressure, nutrient-rich environment of the natural uterus, allowing the baby’s organs to continue developing more naturally outside the body.
One of the most publicized examples of this technology is the ‘BIOBAG’ developed at Children’s Hospital of Philadelphia (CHOP). This system involves placing a premature lamb fetus (a common research model due to similarities with human fetal development) into a sterile bag filled with artificial amniotic fluid. The fetus’s own heart pumps blood through its umbilical cord to a gas exchange unit outside the bag, effectively acting as an artificial placenta, oxygenating the blood and removing carbon dioxide.
Results in animal trials have shown promising outcomes, with lamb fetuses continuing to develop for several weeks within these systems, growing wool and showing increased brain and lung maturation compared to conventional methods. While human trials for this specific system are still a significant way off, this work demonstrates the fundamental viability of supporting life and development outside the conventional womb for a critical period.

The Leap to Full Gestation: Ectogenesis
Supporting a few weeks of premature development is one thing; enabling full gestation from conception to term (around 40 weeks) is an entirely different, monumental challenge. This is the realm of true ectogenesis.
Achieving full ectogenesis requires replicating the complex, dynamic interactions of the uterine environment for the entire nine months. This includes:
- Nutrient and Waste Exchange: A system that can seamlessly provide all necessary nutrients, hormones, and growth factors to the developing embryo and fetus while efficiently removing waste products, mimicking the placenta’s sophisticated function.
- Oxygenation: An artificial placenta capable of handling the increasing oxygen demands of a growing fetus over many months.
- Mechanical Environment: Providing the right physical support, cushion, and possibly even tactile stimulation that the fetus experiences within the natural womb.
- Immune Function: Replicating the crucial role of the maternal immune system in protecting the fetus while preventing rejection.
- Hormonal Regulation: Managing the complex hormonal shifts that govern fetal development and signal the readiness for ‘birth.’
Currently, we are light years away from replicating this level of complexity and duration. The step from supporting a highly developed, late-term fetus for weeks to nurturing an embryo from its earliest stages for months is vast, involving fundamental biological processes that are not yet fully understood or replicable in an artificial system.
Potential Transformations: Reshaping Parenthood and Society
Should full ectogenesis become a reality, its impact on human life and society would be nothing short of revolutionary. The potential benefits are immense, particularly for those facing reproductive challenges.
- Ending Infertility: For individuals and couples struggling with infertility due to uterine factors (absence, damage, disease), ectogenesis could offer a direct path to biological parenthood without the need for surrogacy.
- Eliminating Pregnancy Risks: Many severe health risks associated with pregnancy – preeclampsia, gestational diabetes, ectopic pregnancy, complications during labor and delivery – could potentially be bypassed entirely. This could save countless lives and reduce maternal morbidity globally.
- Medical Interventions: It might allow for intricate medical or genetic interventions on the fetus without impacting the carrying parent’s health.
- Equality in Parenthood: Ectogenesis could offer identical biological parenting opportunities to same-sex male couples or transgender individuals who lack a uterus, fundamentally altering traditional biological constraints on parenthood.
- Shifting Gender Roles: By decoupling gestation from the female body, societal expectations and traditional gender roles surrounding pregnancy, childbirth, and early parenting could be significantly altered.
- Military and Hazardous Environments: Speculatively, it could allow for reproduction without exposing potential parents in hazardous or deployed situations to pregnancy risks.
The possibilities are staggering, offering hope and new avenues for many, while also challenging deeply ingrained biological and societal norms.
The Weighty Debates: Ethics, Law, and Society
As with any technology that touches upon the fundamental aspects of life and reproduction, artificial wombs bring with them enormous ethical, legal, and societal questions. These debates are already beginning, even with the limited current capabilities.
- Status of the Fetus: Does gestation in an artificial environment change the moral or legal status of the fetus? How would this impact abortion rights debates?
- Parental Bonding: How would the absence of physical pregnancy affect the bonding process between parents and child? Would there be unforeseen psychological impacts?
- Accessibility and Equity: Who would have access to this technology? Would it become a tool only for the wealthy, exacerbating existing inequalities?
- Regulation and Oversight: How would such facilities be regulated? What would be the legal framework surrounding conception, development, and ‘birth’ from an artificial womb?
- Defining ‘Birth’: If a baby develops entirely outside a human body, what constitutes the moment or process of ‘birth’?
- Commercialization: Could this technology lead to the problematic commercialization of gestation or even human life?
- The Role of Women: How would the decoupling of gestation from women’s bodies impact women’s roles, identity, and status in society?
These are not simple questions, and finding answers will require extensive public discourse, careful ethical consideration, and robust legal frameworks developed over many years.

Challenges and the Road Ahead
Beyond the ethical minefield, significant technical and practical hurdles remain before full ectogenesis could ever be realized:
- Biological Complexity: Replicating the intricate biological signalling, hormonal milieu, and developmental cues of the uterus for 40 weeks is an immense scientific challenge.
- Scalability: Creating systems capable of supporting thousands or millions of gestations safely and effectively is a massive engineering and logistical task.
- Cost: Developing and maintaining such sophisticated medical technology will undoubtedly be incredibly expensive, at least initially.
- Safety: Ensuring the long-term health and well-being of individuals gestated artificially requires rigorous testing and understanding of potential subtle impacts on development.
- Public Acceptance: Overcoming potential public skepticism and fear surrounding a technology that so fundamentally alters the reproductive process.
Currently, research remains focused on improving outcomes for premature infants. The path to full ectogenesis is long, paved with significant scientific, engineering, and societal challenges.
FAQs About Artificial Wombs and Ectogenesis
Q: Are artificial wombs currently used for full human gestation?
A: No. Artificial wombs are not currently capable of supporting full human gestation from conception to birth. Current research focuses on supporting extremely premature infants for a limited period to improve their outcomes.
Q: What is the difference between an artificial womb and ectogenesis?
A: An artificial womb is a general term for any device or system designed to support fetal development outside the body. Ectogenesis specifically refers to the process of gestating an organism entirely outside of a living body, ideally from conception to term.
Q: Can artificial wombs replace surrogacy?
A: Not currently. However, if full ectogenesis becomes possible, it could potentially offer an alternative path to biological parenthood for those who might otherwise need surrogacy due to uterine factors.
Q: What are the biggest challenges to developing full ectogenesis?
A: The challenges are vast, including replicating the complex biological and hormonal environment of the uterus, ensuring long-term healthy development, technical engineering hurdles, cost, and navigating profound ethical, legal, and societal questions.
Q: Is this technology safe?
A: The systems used for premature infants are undergoing rigorous testing and refinement. Full ectogenesis is so far from reality that safety hasn’t been tested, but any future development would require extensive research to ensure the safety and long-term health of children gestated artificially.
Charting Worlds Apart
From the most ancient, intimate form of nurturing life, humanity is charting a course towards possibilities that were once confined to imagination. Artificial wombs, currently serving as a vital bridge for the most vulnerable premature lives, hint at a future where science could potentially offer entirely new beginnings, weathering the storms of biological limitation and risk.
This journey from the familiar embrace of nature’s oldest art to science charting worlds apart is just unfolding. It prompts us to pause, consider, and engage in the vital conversations needed to navigate this profound shift. What possibilities and questions are buzzing in your mind?
Don’t keep these complex ideas gestating alone! Like this post if it got you thinking, and subscribe to stay with us as we continue to explore the frontiers of tomorrow’s technology.





