Imagine a world where a tiny, subtle sign of illness, years before you felt anything amiss, was caught not by chance, but by design. What if technology could peer into the intricate details of your body and spot sickness *years* before a doctor could detect it using traditional methods? This isn’t science fiction; it’s the exciting frontier of Artificial Intelligence in healthcare.
Medical scans—MRIs, CTs, X-rays—are treasure troves of data. They capture incredible detail about our internal landscape. But within that vast ocean of information, finding those *tiny*, early warning signs, say, a microscopic tumor just beginning its journey, is incredibly tough. It’s a task that demands extreme focus, experience, and frankly, a bit of luck, even for the most seasoned medical experts. Early detection is often the key to successful treatment and survival, but finding that ‘needle in a haystack’ early on has always been a significant challenge.
That’s exactly where Artificial Intelligence is stepping in, promising to revolutionize how we approach proactive health and disease diagnosis. Think of AI as giving doctors not just a helping hand, but a kind of ‘superhero vision’. If the idea of AI seeing the unseen blew your mind, you might want to see this quick visual take on it:
So, how does this powerful ‘early warning radar’ actually work?
Table of Contents
The Challenge of Spotting Early Signs
Before we dive into AI’s role, let’s understand the complexity. A single CT scan can contain thousands of individual images. A radiologist reviews these images, looking for anomalies, patterns, and changes. Early-stage diseases, particularly cancers, often manifest as extremely subtle changes – perhaps a slight difference in tissue density, an irregular shape only a few pixels wide, or a pattern that only becomes significant when viewed in conjunction with other, seemingly unrelated, findings across multiple slices of a scan.
Identifying these minute details requires immense cognitive load, expertise, and concentration. Over long shifts, even the best radiologists can face fatigue, and the sheer volume of scans needing review globally is staggering. This human limitation, while understandable, can unfortunately lead to delayed diagnoses.
AI: Learning to See the Unseen
Artificial Intelligence, specifically a branch called Machine Learning, particularly Deep Learning and Convolutional Neural Networks (CNNs), is exceptionally good at pattern recognition in images. The key difference from the human eye is scale and consistency.
AI algorithms are trained on massive datasets – sometimes millions of medical images, meticulously labeled by human experts indicating the presence or absence of disease, and marking the locations of abnormalities. Through this training, the AI learns to identify patterns, textures, shapes, and spatial relationships that are statistically correlated with specific diseases.
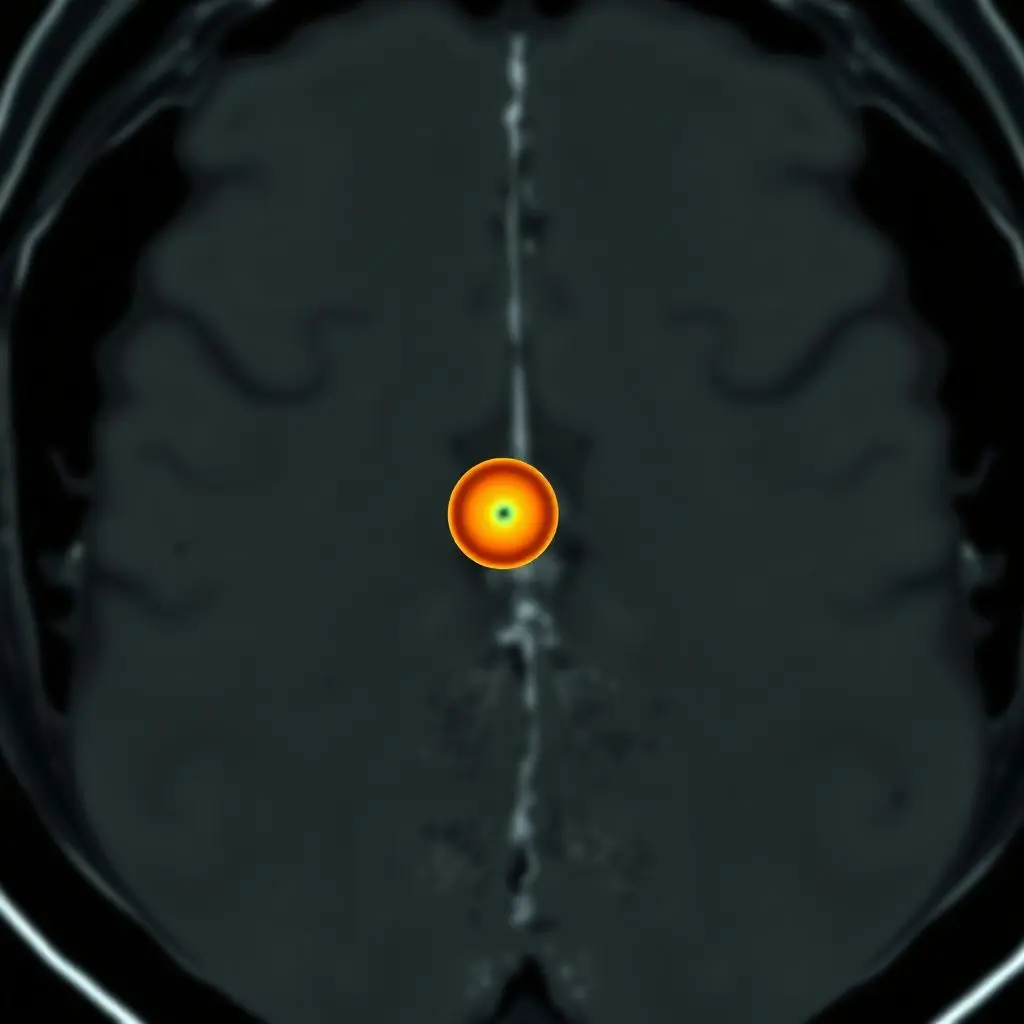
Crucially, AI can process and analyze every single pixel and its relationship to surrounding pixels across an entire scan volume simultaneously and consistently, something impractical for a human. It can pick up on micro-calcifications in mammograms too small to be immediately obvious, detect subtle lung nodules on CTs that might be missed on first pass, or identify early signs of neurological conditions in brain MRIs.
Real-World Impact: Spotting Cancer Earlier
One of the most prominent applications is in cancer screening. Studies have shown AI models achieving performance comparable to, and in some cases exceeding, human accuracy in detecting certain cancers from scans:
- Mammography: AI is being used to analyze mammograms for signs of breast cancer, often identifying suspicious areas that warrant further investigation earlier than traditional methods alone. Some AI systems can flag these potential issues years before they would typically be noticeable or large enough to be clinically significant via standard screening protocols.
- Lung Cancer: Analyzing low-dose CT scans of the lungs, AI can help detect small pulmonary nodules that could be early signs of lung cancer. Given the aggressive nature of many lung cancers, catching them when they are small and localized dramatically increases survival rates.
- Prostate Cancer: AI is being explored to help interpret MRI scans of the prostate, identifying suspicious lesions that may indicate cancer and helping guide biopsies.
- Other Cancers: Research is ongoing into applying AI to detect signs of other cancers, including colorectal polyps from CT colonography, pancreatic cysts from abdominal scans, and even certain types of skin cancer from dermatological images.
The potential here isn’t just about finding existing disease; it’s about finding it at its absolute earliest, most treatable stage.
AI: An Essential Tool, Not a Replacement
It’s vital to understand that AI in this context is designed to be a powerful *assistive tool* for medical professionals, not a substitute. AI doesn’t understand the full clinical context of a patient – their history, symptoms, lifestyle, and other test results. It identifies potential red flags based purely on image analysis.
When an AI algorithm flags a suspicious area, it alerts the radiologist or clinician. The human expert then reviews the AI’s findings alongside the rest of the scan and the patient’s information to make a final diagnosis and treatment plan. AI helps prioritize cases, highlight difficult-to-see anomalies, and provide a ‘second opinion’ based on objective pattern recognition.
This collaborative approach, often termed ‘AI-assisted diagnosis’, leverages the strengths of both humans and machines: AI for tireless, granular pattern detection across massive datasets, and humans for nuanced interpretation, clinical judgment, and patient care.
Challenges on the Horizon
While incredibly promising, the path to widespread AI integration in early detection isn’t without hurdles:
- Data Bias: AI models are only as good as the data they’re trained on. If training data isn’t representative of diverse populations, the AI might perform poorly on certain demographic groups.
- Interpretability: Understanding *why* an AI flagged something can be complex (‘black box’ problem). Doctors need to trust and understand the basis of the AI’s suggestions.
- Regulatory Approval: Medical AI systems need rigorous testing and approval from health authorities before widespread clinical use.
- Integration: Seamlessly integrating AI tools into existing clinical workflows and IT systems is a significant practical challenge.
- Privacy: Handling vast amounts of sensitive patient data for training and operation requires robust security and privacy measures.
Addressing these challenges is crucial for the successful and ethical deployment of AI in healthcare.

Looking Ahead: The Ultimate Early Warning Radar
The vision of AI acting as an ultimate early warning radar for health is rapidly becoming a reality. As AI models become more sophisticated, trained on even larger and more diverse datasets, and integrated with other forms of health data (like genetic information, wearable sensor data, and clinical history), their ability to detect the earliest whispers of disease will only improve.
This isn’t just about finding illness sooner; it’s fundamentally shifting healthcare towards a more proactive, preventive model. By identifying potential health issues at their nascent stage, before symptoms even appear, AI can enable earlier interventions, less invasive treatments, and ultimately, save countless lives. It empowers both patients and doctors with the knowledge and tools to act decisively at the most opportune moment.
Frequently Asked Questions (FAQs)
Will AI replace radiologists?
No, the current consensus among experts is that AI will augment, not replace, radiologists. AI can efficiently process and flag potential issues in scans, but human radiologists are essential for nuanced interpretation, clinical context, patient interaction, and making the final diagnosis.
How accurate is AI at detecting diseases?
Accuracy varies depending on the specific disease, the quality and size of the training data, and the AI model used. In some specific tasks, AI performance has reached or even surpassed human accuracy, but it’s crucial to validate these systems rigorously in real-world clinical settings. AI is currently best used as a tool to assist humans, improving overall diagnostic efficiency and accuracy.
What types of medical scans can AI analyze?
AI is being developed to analyze a wide range of medical images, including CT scans, MRIs, X-rays, mammograms, ultrasounds, pathology slides, retinal images, and dermatological photographs.
Is my data safe when used for training AI?
Reputable institutions and developers training medical AI use anonymized or de-identified data whenever possible and comply with strict data privacy regulations like HIPAA (in the US) or GDPR (in Europe). Data security is a critical concern that needs to be addressed with robust protocols.
When will AI be widely used in hospitals for early detection?
AI tools are already being used in some hospitals for specific applications, particularly in radiology. Widespread adoption depends on regulatory approval, successful integration into clinical workflows, and building trust among medical professionals and patients. Progress is rapid, and adoption is expected to grow significantly in the coming years.