Imagine this: You or a loved one needs a vital organ transplant. Instead of entering a waiting list that stretches months, sometimes years, you could potentially have that organ manufactured specifically for you. It sounds like something straight out of science fiction, doesn’t it?
Tragically, millions around the globe face the stark reality of critical waiting periods for life-saving organ transplants. The demand far outweighs the available supply from generous donors. But what if there was another way? What if we could literally ‘print’ the organs we need?
Incredible progress is being made in the fascinating field of 3D bioprinting, hinting at a future where organ shortages could become a relic of the past. Let’s dive into this revolutionary technology. To get a quick, mind-blowing glimpse, check out this short video:
Table of Contents
What Exactly is 3D Bioprinting?
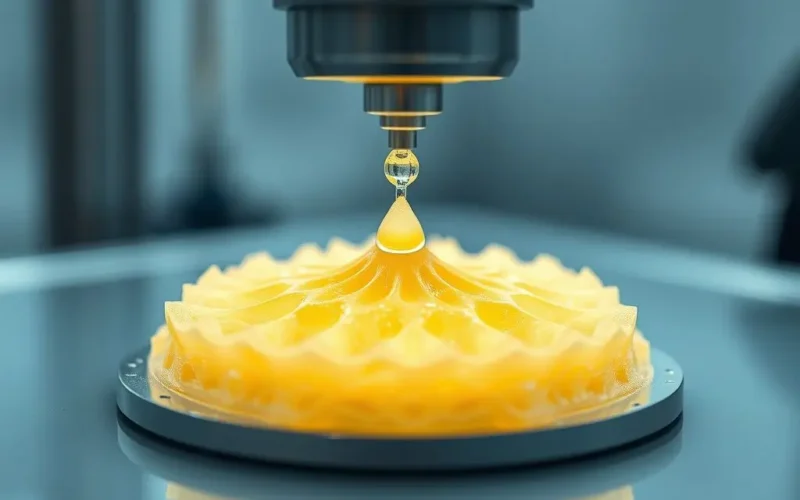
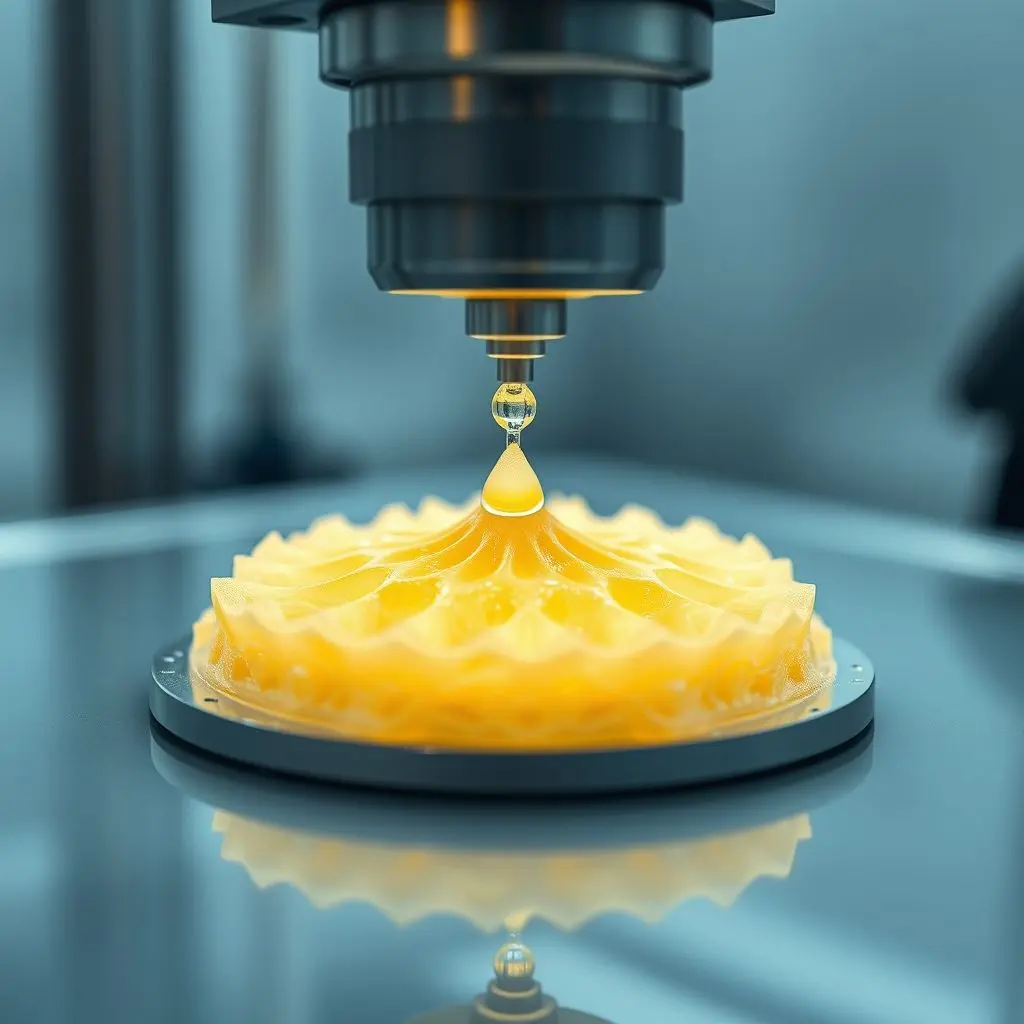
When we talk about 3D bioprinting, we’re not referring to the plastic-extruding printers you might see making prototypes or trinkets. These are sophisticated machines engineered to handle something far more delicate and complex: living cells and biological materials.
Think of it as manufacturing, but with biological building blocks. A 3D bioprinter works by layering these biological ‘inks’ – often referred to as bioinks – with immense precision, drop by tiny drop or line by line, following a digital blueprint. This blueprint is typically created from scans of real organs or tissues.
The Vital Ingredients: Bioinks and Cells
At the heart of bioprinting are the materials it uses. Unlike conventional 3D printing which uses plastics or metals, bioprinting requires substances that are biocompatible and can support cell life. This is where bioinks come in.
Bioinks are complex formulations that can contain:
- Living Cells: These are the stars of the show. They can be patient-specific cells (like stem cells derived from the patient) or cells from other sources, carefully prepared for printing.
- Biomaterials: These provide the structural support, acting like a scaffolding (or extracellular matrix) that the cells need to grow, differentiate, and organize into functional tissue. Common biomaterials include hydrogels made from natural substances like alginate or collagen, or synthetic polymers designed to be non-toxic and biodegradable.
The bioink must be printable (viscous enough to hold shape but fluid enough to pass through the printer nozzle), compatible with cell survival, and capable of mimicking the natural environment of the tissue being printed.
The Layering Process: Building Tissues from Scratch
The bioprinting process itself is akin to building a miniature, biological structure layer by intricate layer. It typically involves:
- Design: Creating a detailed 3D model of the desired tissue or organ using imaging data.
- Bioink Preparation: Mixing the cells with the chosen biomaterial to create the printable bioink.
- Printing: The bioprinter precisely deposits the bioink onto a substrate according to the 3D model. Different printing techniques exist, including extrusion-based, inkjet-based, and laser-assisted bioprinting, each suited for different cell types and tissue structures.
- Maturation (Post-Printing): This is a crucial step. After printing, the structure is typically placed in a bioreactor – a controlled environment mimicking the body’s conditions (temperature, nutrients, growth factors). Here, the cells proliferate, differentiate, and reorganize to form functional tissue. This can take days, weeks, or even months depending on the complexity.
The “Why”: Why Bioprinting Holds Immense Promise
The potential benefits of 3D bioprinting in regenerative medicine, particularly for organ transplantation, are revolutionary:
- Addressing the Donor Shortage: This is perhaps the most significant driver. Bioprinting offers the possibility of creating organs on demand, potentially eliminating the need for waiting lists and the tragic loss of life due to organ scarcity.
- Reduced Risk of Rejection: By using a patient’s own cells, the bioprinted organ would be genetically identical to the recipient. This could drastically reduce or even eliminate the need for powerful immunosuppressant drugs, which have significant side effects and risks.
- Customization and Perfect Match: Organs could be printed to the exact size and shape needed for an individual patient, based on their unique anatomy.
- Reduced Procedure Risks: A bioprinted organ, being a perfect match, might lead to simpler surgical procedures and faster recovery times compared to traditional transplants.
- New Opportunities for Research: Printed tissues and mini-organs can be used for drug testing and disease modeling, providing more accurate results than traditional methods and reducing the need for animal testing.

The Hurdles: The Long Road to Functional Organs
While the potential is vast, printing a fully functional organ is an incredibly complex undertaking and remains a significant scientific and engineering challenge. Some of the major hurdles include:
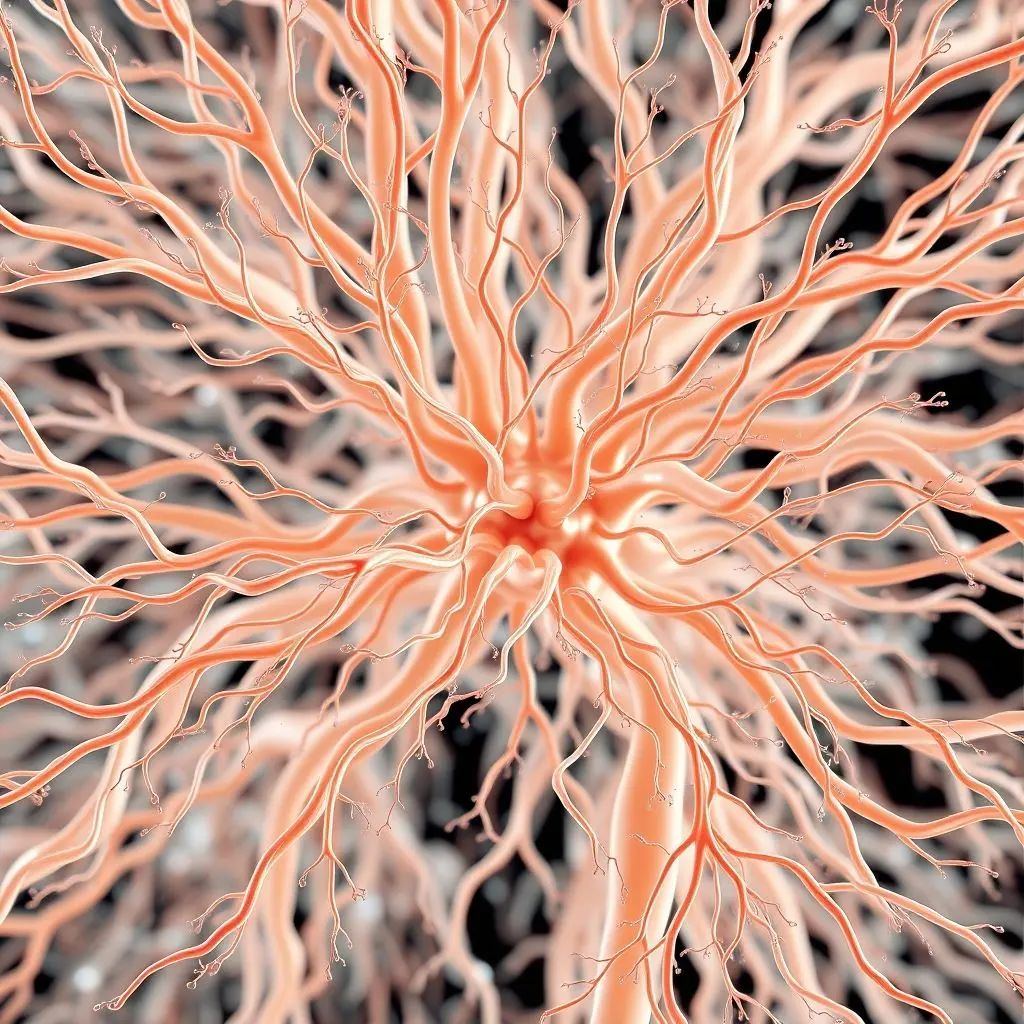
- Vascularization: Organs are densely packed with blood vessels that supply oxygen and nutrients and remove waste. Creating this intricate network within a printed structure is extremely difficult but absolutely vital for the survival and function of large tissues. Without a working vascular system, the cells in the interior would quickly die.
- Cell Viability and Function: Ensuring cells survive the printing process and then mature into the correct cell types that behave exactly as they would in a native organ is challenging.
- Structural Integrity: Printed tissues need to have the mechanical strength and flexibility of natural organs.
- Complexity of Organs: Organs like hearts or kidneys are not just blocks of cells; they have incredibly complex 3D architectures, multiple cell types arranged in specific ways, and integrated functionality. Replicating this is a monumental task.
- Regulatory Approval and Scalability: Even if successful in the lab, getting these technologies approved for human use and scaled up for widespread availability will require navigating complex regulatory pathways and manufacturing challenges.
- Cost: Initially, the technology is likely to be prohibitively expensive.
Progress in the Labs: What’s Being Printed Now?
Despite the challenges, the progress being made is truly remarkable. Researchers aren’t yet printing full, ready-to-transplant hearts or livers for widespread use, but significant milestones are being achieved:
- Functional Skin: Printing layers of skin tissue is one of the more advanced applications, holding promise for treating burns and other injuries.
- Miniature Organs (Organoids): Scientists are printing small, simplified versions of organs like mini-kidneys, livers, and hearts. While not transplantable in humans yet, these are invaluable tools for studying disease, testing drugs, and understanding tissue development.
- Blood Vessels and Tubes: Successfully printing complex vascular structures is a major focus, as it’s critical for supporting larger printed tissues.
- Cartilage and Bone: Printing tissues for musculoskeletal repair is also showing promise.
These lab-scale successes, while not full organs, represent critical steps forward, proving the viability of the core concepts and tackling specific components of the larger challenge.
The Road Ahead: A Glimpse into the Future
The ultimate goal is clear: to print fully functional, transplantable organs on demand. While we are still some years away from this becoming a routine clinical reality, the trajectory of research is exciting. The field of 3D bioprinting is converging with advancements in stem cell technology, materials science, and robotics to push the boundaries of what’s possible.
Imagine a future where personalized organs are available when needed, manufactured from your own cells, eliminating the agonizing wait and the lifelong need for immunosuppressants. This technology could fundamentally transform healthcare, extending and improving countless lives.
Frequently Asked Questions About 3D Bioprinting Organs
Here are some common questions people ask about this cutting-edge field:
Q: Is it possible to print a full, working human organ right now?
A: Not yet. While researchers are printing complex tissues and miniature organs for research purposes, printing a full-sized, functional organ suitable for human transplantation that includes a working vascular system and all necessary cell types in the correct architecture is still a future goal. It’s a major focus of research globally.
Q: How long does it take to print a tissue or organ?
A: The printing itself can take anywhere from minutes to hours, depending on the size and complexity. However, the post-printing maturation process, where cells grow and organize into functional tissue, can take much longer – days, weeks, or even months in a bioreactor before it could potentially be ready for use (even in a research context).
Q: What kinds of cells are used in bioprinting?
A: A variety of cell types can be used, including patient-derived cells (like induced pluripotent stem cells (iPSCs) which can be differentiated into various tissue-specific cells), adult stem cells, or even primary cells directly isolated from tissue samples.
Q: Will bioprinted organs look and feel like real organs?
A: The goal is to replicate the structure and function of natural organs as closely as possible. While the early stages might involve scaffolds that differ slightly, the aim is for the final mature tissue to mimic the native organ’s properties.
Q: Is this technology safe?
A: Safety is paramount. Extensive research and testing are required before any bioprinted tissue or organ can be considered for human use. Challenges include ensuring the long-term viability and function of the printed cells, preventing tumor formation, and ensuring the biomaterials used are completely safe and biocompatible within the body.
The Horizon of Regenerative Medicine
The concept of printing organs is undeniably mind-blowing, a testament to human ingenuity pushing the boundaries of biology and engineering. While significant challenges remain, the rapid pace of innovation in 3D bioprinting paints a hopeful picture. We are moving towards an era where regenerative medicine could provide solutions that were once unimaginable, potentially offering a lifeline to those waiting for a second chance at health.